
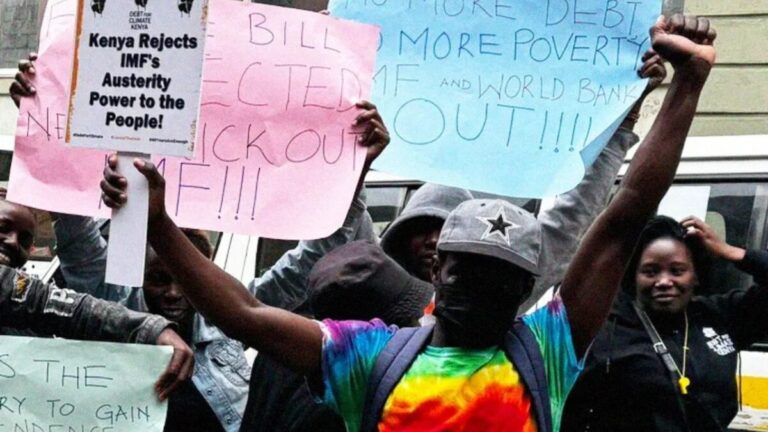
In Kenya, 69% of women with fistulas surveyed reported at least 2 delays in receiving care when they experienced obstructed labor. (Photo/ Mwiri Stephen).
By Daisy Okiring and Nguvu Collective
Today, as we mark the International Day to End Obstetric Fistula, Kenya joins the global community in acknowledging a crisis that has for too long existed in silence. In hospitals meant to nurture life, thousands of Kenyan women experience childbirth not as a moment of joy, but as a harrowing passage marked by neglect, abuse, and irreversible injury.
Two devastating and interconnected crises haunt Kenya’s maternal healthcare system: obstetric fistula, a severe childbirth injury caused by prolonged obstructed labor, and obstetric violence, a systemic form of gender-based mistreatment within health facilities. Though rarely addressed in the national spotlight, these issues disproportionately affect Kenya’s most vulnerable women—young girls, the disabled, and those living in rural poverty.
According to the Ministry of Health, over 3,000 new cases of obstetric fistula are reported in Kenya each year. Yet UNFPA estimates that less than 8% of these women receive timely, life-restoring treatment.
The Nurse Who Wasn’t Heard
Deborah Monari’s story illustrates the paradox of a broken system from within. A registered nurse dedicated to care, she suddenly found herself on the other side of the hospital bed—experiencing misdiagnoses, dismissal, and emotional trauma when she sought help for persistent neurological symptoms.
“I saw over five doctors, and none of them took me seriously,” she recalls. “I was told it was stress. I knew it was more.”
Only when she sought help in India was the truth uncovered—a brain tumor that required immediate surgery. Her experience led to a revelation: if this could happen to her, a healthcare professional, what were ordinary Kenyan women enduring?
Also Read: Kenya Forgotten Schools: Education in arid regions
That realization fueled her campaign. Deborah launched a national petition demanding the establishment of Patient Rights Committees in all Kenyan hospitals. With over 1,000 signatures and counting, she hopes these watchdog bodies will transform medical accountability.
Her efforts are supported by the Nguvu Change Leaders Collective, a UKAID-backed initiative empowering grassroots changemakers to reform health and social justice systems in Kenya. “We need to ensure that no woman walks through a hospital door and walks out worse than she came in,” Deborah says.

“Being a nurse didn’t protect me from medical negligence.” Deborah Monari, a registered nurse now campaigns for patient rights after surviving a harrowing misdiagnosis. (Photo/Nguvu Collective).
Disability and Disrespect in Delivery Rooms
For Josephine Mwende Kamene, childbirth meant navigating not just contractions, but discrimination. Living with cerebral palsy, she faced skepticism from the moment she arrived at the maternity ward. Staff questioned her decision to become a mother. Equipment was inaccessible. Pain relief was withheld.
“We are treated like second-class citizens,” Josephine says. “Even as we bring life into the world, our dignity is denied.”
Josephine is the founder of AbleRise Africa Society, a community-based organization dedicated to the rights of women with disabilities. Through advocacy and storytelling, she’s amplifying the experiences of those too often left out of reproductive health conversations.
Like Deborah, Josephine is a Nguvu Change Leader. Her petition calls for accessible consultation rooms, staff sensitivity training, and toll-free reporting lines for hospital abuse. “We’re not just demanding services,” she says. “We’re demanding to be seen as women—capable, worthy, and human.”

Josephine Mwende stands tall as an advocate for disability rights, redefining what it means to be a mother in a system that doubted her worth. (Photo/Nguvu Collective.)
The Global Burden of Fistula
Fistula is a deeply preventable injury, yet it continues to scar the lives of thousands. Globally, the World Health Organization estimates that up to 100,000 women develop obstetric fistula each year. In Kenya, young girls—often victims of child marriage—are especially at risk, with prolonged, unattended labor causing devastating damage.
According to Amref Health Africa, fewer than 20 hospitals in Kenya offer fistula repair surgery. Amref has supported more than 10,000 fistula operations, but demand far outpaces supply.
“Obstetric fistula is not just a medical issue—it is a symbol of failed systems and forgotten women,” says UNFPA Kenya. “It is rooted in gender inequality and broken access to maternal care.”

Fistula survivors often live in shame and isolation—abandoned by health systems and blamed by society for injuries they never chose. (Photo/OSU).
Obstetric Violence: The Unseen Epidemic
Beyond fistula lies a broader, more insidious problem: obstetric violence. A 2022 study by the African Population and Health Research Center (APHRC) found that 37% of women in Kenya experienced some form of mistreatment during childbirth. This includes physical abuse, verbal insults, non-consensual procedures, and abandonment.
Also Read: Inside the power struggles over UoN’s Sh211 billion empire
“Too often, women give birth in fear—not of the pain, but of how they’ll be treated,” says Dr. Christine Owino, an OB-GYN based in Nairobi.
Women with disabilities report even more severe treatment. Many are denied pain medication or have decisions made without their consent. Josephine recalls, “Some are sterilized without their knowledge. Others are told they shouldn’t have children at all.”

Behind closed doors in maternity wards, women are too often silenced, ignored, or abused by the very people entrusted to help them. (Photo/LinkedIn).
Nguvu Change Leaders: Voices for Justice
The Nguvu Change Leaders Collective is building a new future—one led by survivors, advocates, and community champions. The initiative, powered by UKAID, Well Made Strategy, and Voice Global, supports over 60 Kenyan leaders tackling issues from maternal health and disability inclusion to mental health and gender-based violence.
Nguvu doesn’t just amplify stories—it equips its leaders with tools, platforms, and networks to influence change.
A Future Rooted in Respect
What would a maternal healthcare system built on respect look like?
According to Deborah, it would begin with listening. “Every woman should feel safe and valued when giving birth,” she says.
Josephine envisions fully accessible clinics, well-trained staff who treat disability with dignity, and empowered patients who know their rights.
Together, they agree that healthcare reform must go beyond infrastructure. It must confront societal bias, protect patients from abuse, and ensure that no woman—no matter how poor, young, or different—is left behind.
Also Read: How Kenyan girls are lured into Russian war
Today, We End the Silence
Today, on May 23—the International Day to End Obstetric Fistula, Kenya has a choice: to continue looking away, or to stand with women like Deborah and Josephine, who are bravely transforming their wounds into weapons for justice.
Their message is unyielding: maternal healthcare must heal, not harm. And change is no longer a request—it’s a demand echoing from every woman silenced, every fistula survivor, every disabled mother told she didn’t belong.
“We will not wait to be saved,” says Deborah. “We are the ones we’ve been waiting for.”



3 thoughts on “Obstetric Fistula: A tragedy haunting Kenyan maternity wards”
Comments are closed.